Intravenous (IV) therapy is a critical skill for nurses, central to the delivery of fluids, medications, electrolytes, and nutrients directly into the bloodstream. This method ensures rapid and effective treatment in various clinical settings, ranging from emergency rooms to outpatient care. For nurses, understanding IV therapy is essential—not only in performing the technical aspects of intravenous insertion but also in drug calculations, preventing complications, and educating patients.
This guide will cover everything a nurse needs to know about IV therapy, including types of IV therapy, drug calculations, nursing responsibilities, patient safety protocols, and essential best practices.
What is IV Therapy?
IV therapy is the process of administering substances directly into a vein. The substances can include medications, fluids, vitamins, and electrolytes, which bypass the digestive system and deliver therapeutic effects more rapidly. This is crucial for patients who need immediate intervention, especially in cases of dehydration, infection, surgery recovery, or when medications must be given quickly.
Because IV therapy is so effective at providing fast and controlled treatment, it is widely used in healthcare settings for:
- Emergency care: When quick hydration or drug delivery is needed.
- Long-term therapy: For chronic conditions requiring regular treatment.
- Nutritional support: For patients who are unable to eat or absorb nutrients orally.
Why IV Therapy is Critical in Nursing
For nurses, IV therapy is a key component of patient care, offering several benefits:
- Rapid therapeutic effects: Medications and fluids reach the bloodstream immediately, providing fast relief for patients in critical situations.
- Control over dosage: IV therapy allows for precise control over the rate and amount of medication or fluids being administered, ensuring safety and effectiveness.
- Flexible use: IV therapy can be tailored to meet the specific needs of each patient, from hydration to medication administration and nutritional support.
- Multifunctional: IV therapy can be used for rehydration, blood transfusions, delivering pain medications, administering antibiotics, and even chemotherapy.
Nurses need to be proficient not only in inserting and maintaining IV lines but also in calculating drug doses accurately and recognizing potential complications. IV therapy is more than a technical procedure—it requires critical thinking, patient monitoring, and adherence to safety protocols.
Types of IV Therapy
Understanding the various types of IV therapy is crucial for choosing the right treatment approach for each patient. Each type has its own specific uses, risks, and nursing considerations.
1. Peripheral IV Therapy
Peripheral IVs are the most common type of intravenous access and are used for short-term treatments. The catheter is typically inserted into a small vein, usually in the hand, wrist, or forearm.
- Common Uses: Administering fluids for dehydration, providing medications such as antibiotics, or infusing blood products.
- Duration: Usually in place for up to 72–96 hours, after which the IV site should be rotated to prevent complications like phlebitis or infection.
Nursing Considerations:
- Nurses must monitor for signs of infiltration (when the fluid leaks into surrounding tissues), phlebitis (vein inflammation), and infection. Regular checks of the IV site are essential to detect these issues early.
2. Central IV Therapy
Central venous catheters (CVCs) are used for patients requiring long-term IV therapy or who have poor peripheral access. These catheters are inserted into large central veins, usually near the heart (internal jugular, subclavian, or femoral veins).
- Types of Central Lines:
- PICC (Peripherally Inserted Central Catheter): Inserted in the arm and threaded to a central vein near the heart. Ideal for long-term therapies like chemotherapy or prolonged antibiotic administration.
- Implanted Ports: Surgically placed under the skin, these are typically used for patients who require long-term, intermittent access, such as cancer patients receiving chemotherapy.
- Tunneled Catheters: These are inserted through a small incision in the chest and tunneled under the skin to a central vein. They are used for long-term treatments such as dialysis or chemotherapy.
Nursing Considerations:
- Central lines require more complex care, including sterile dressing changes, regular flushing with heparin to maintain patency, and monitoring for potential complications such as catheter-related bloodstream infections (CRBSIs) or blood clots.
3. Total Parenteral Nutrition (TPN)
TPN is a specialized form of IV therapy that provides all the nutrients a patient needs when they are unable to take food or nutrients by mouth or through enteral feeding (via the digestive tract).
- Components of TPN: TPN solutions contain carbohydrates, proteins, fats, electrolytes, vitamins, and trace elements, all tailored to meet the patient’s specific nutritional requirements.
- Indications: Patients with bowel obstructions, Crohn’s disease, or severe malnutrition may require TPN.
Nursing Considerations:
- Strict monitoring of electrolytes, blood glucose levels, liver function, and renal function is crucial. TPN can cause complications such as hyperglycemia or liver dysfunction if not carefully managed.
4. IV Medication Therapy
IV medication therapy is the intravenous administration of drugs, which ensures rapid delivery of the medication into the bloodstream. It is commonly used for:
- Antibiotics: Treat infections with immediate therapeutic effects.
- Analgesics: Administer pain relievers such as morphine or fentanyl, especially in postoperative or trauma care.
- Anticoagulants: Drugs like heparin are used to prevent or treat blood clots.
- Chemotherapy drugs: For the treatment of cancer.
Nursing Considerations:
- Accurate drug calculations, administration rates, and careful monitoring of the patient for adverse reactions or side effects are essential.
Drug Calculations for IV Therapy
Accurate drug calculation is one of the most critical aspects of IV therapy. Nurses must ensure the correct dosage, flow rate, and volume are administered to avoid medication errors, which can have serious consequences for patients. Below are essential calculations nurses need to master for safe IV therapy.
1. Calculating IV Flow Rate (gtt/min)
The IV flow rate is calculated in gtt/min (drops per minute) using the following formula:
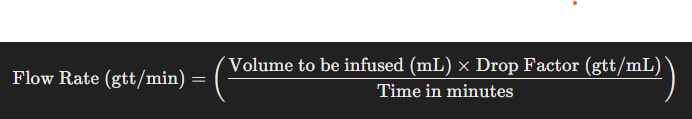
- Volume to be infused: The total amount of fluid to be delivered (in mL).
- Drop factor: This is specific to the IV tubing used (commonly 10, 15, or 20 gtt/mL).
- Time: The total time of infusion (in minutes).
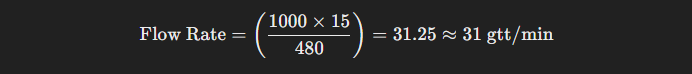
Example:
- Volume to be infused = 1000 mL
- Drop factor = 15 gtt/mL
- Time = 8 hours (480 minutes)
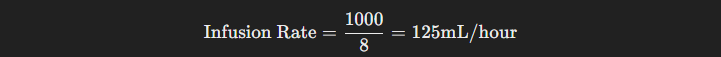
2. Calculating IV Infusion Rate (mL/hour)
To calculate the infusion rate in mL/hour, use the following formula:

Example:
- Volume to be infused = 1000 mL
- Time = 8 hours
3. Weight-Based Dosing
Some medications are dosed based on a patient’s weight, particularly in pediatric or critical care settings. The formula is:
Example:
- Patient’s weight = 70 kg
- Prescribed dose = 2 mg/kg
Nursing Responsibilities in IV Therapy
The nurse’s role in IV therapy goes beyond simply administering fluids or medications. Nurses must ensure the safety, efficacy, and comfort of the patient throughout the process. Here are key nursing responsibilities when performing IV therapy:
1. Pre-Insertion Assessment
Before inserting an IV, nurses must evaluate the patient’s clinical status, including:
- Patient history: Any history of allergies, previous complications with IV therapy, and current medications should be reviewed.
- Vein selection: Assess the patient’s veins to choose the most appropriate site, considering factors such as hydration status, visibility of veins, and the patient’s overall condition.
- Patient education: Inform the patient about the procedure, its purpose, and what to expect during IV therapy.
2. Inserting the IV and Maintenance
- Aseptic technique: Strict aseptic technique must be followed to prevent infection.
- Proper insertion: The insertion of the catheter should be performed with minimal trauma, ensuring the patient’s comfort and minimizing complications.
- Monitoring the infusion site: Regularly assess the IV site for any signs of complications such as phlebitis, infiltration, or infection.
3. Complication Management
Recognizing and responding to IV therapy complications is critical
for patient safety. Common complications include:
- Infiltration: Fluid leaks into the surrounding tissue, causing swelling and discomfort. The infusion must be stopped immediately, and the catheter relocated.
- Phlebitis: Inflammation of the vein, marked by redness, warmth, and tenderness along the vein.
- Extravasation: Leakage of a vesicant drug into surrounding tissues, which can cause severe tissue damage.
- Infection: Any signs of infection at the IV site should prompt immediate removal of the catheter and initiation of treatment.
4. Patient Education
Effective patient education is key to ensuring patients understand their IV therapy and can report any issues such as discomfort, swelling, or redness. Nurses should explain the purpose of the IV therapy, how long it will take, and what the patient should expect during and after the procedure.
Potential Complications in IV Therapy
While IV therapy is generally safe when performed correctly, complications can arise. Nurses must be vigilant in preventing and recognizing these complications, including:
- Air Embolism: A rare but potentially life-threatening complication that occurs when air enters the bloodstream. Nurses should ensure IV tubing is properly primed to prevent air bubbles.
- Fluid Overload: Administering too much fluid, especially in patients with heart or kidney conditions, can lead to complications like pulmonary edema or heart failure. Nurses should monitor fluid intake and output carefully.
- Electrolyte Imbalances: Infusing electrolyte solutions (e.g., saline or potassium) requires careful monitoring of serum electrolyte levels to prevent complications such as hyperkalemia or arrhythmias.
For nurses, mastering IV therapy is essential for safe, effective patient care. From selecting the correct IV access to performing accurate drug calculations and monitoring for complications, nurses play a critical role in ensuring the success of IV therapy. By following best practices, maintaining vigilance, and providing thorough patient education, nurses can help improve outcomes and ensure the safety and comfort of their patients during IV therapy.